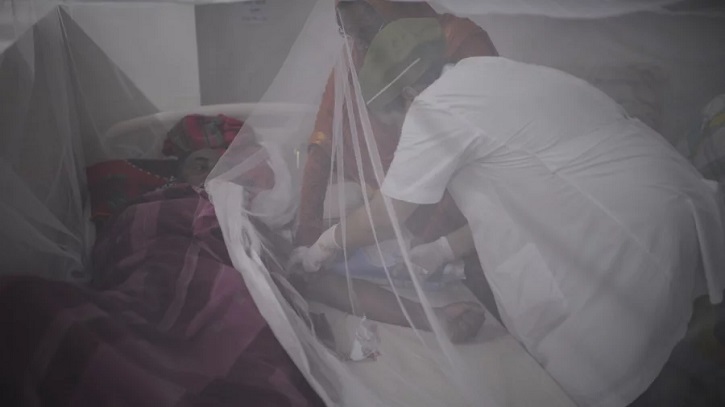
This has probably been the worst month in the history of dengue cases in Bangladesh. The spike came earlier than usual, and the number of deaths is at its highest by this time of the year. Just like other infectious diseases, we needed to break the cycle by eliminating the source of the infection.
In this case, since the culprit is a flying organism that is breeding around us and feeding on us, the paramount objective is to control these vectors. To do this well, a three-pronged approach might work, provided it is executed smartly:
- First, the authorities in charge of mosquito control need extensive understanding of the nature of Aedes aegypti mosquitoes and the time-sensitive relationship of the vector to weather which is altering due to climate change
- Second, dissemination of updated clinical protocol to manage new symptoms and detecting the dominant variant of the season
- Third, establishing a mapping system to identify the locations of the dengue infested areas to take targeted action
What is the nature of Aedes aegypti and virus transmission?
The virus propagation is a vicious cycle entirely depending on the female Aedes aegypti mosquito. It gets infective seven days after biting a dengue positive person and then transmits the virus directly by biting and indirectly by passing the virus down to its eggs. This is a pest that lives close to human habitation with a life span of two weeks, and rests indoors in dark areas to remain protected from wind and predators.
These ankle biters get attracted to carbon dioxide, sweat, and heat emanating from the human body and bite mostly two hours after dawn and two hours before dusk. After feeding on human blood, it finds artificial domestic containers to lay eggs on the inside of them. In its lifetime it produces hundreds of eggs in three to five batches at different sites.
The eggs are dirty looking, sticky, and can dry up to survive from nine months to year. They hatch when covered with little water to the larval stage, and even the larva can remain in a hibernation state for some time. Before flying off as an adult mosquito, both the larvae and pupae live in water and are visible. This whole cycle of hatching to flying takes only seven to ten days but it is dependent on ideal weather conditions and till that happens, the virus is ensconced within the hardy eggs.
What is the correlation with weather, why is it not breeding all the year round and how is it migrating to different parts of the country?
Aedes is an urban mosquito that thrives in densely populated places having less than perfect water supply, sanitation, and waste management. The apparent challenge in controlling the mosquito population might indicate that Aedes can fly fast and travel great distances akin to a jet engine. Surprisingly, unlike other mosquito species that can fly miles, Aedes has a flying range of only a few hundred feet to a maximum of 400m. However, this vector does travel far to migrate to new places but that is attributed to its ability to hitch on suitcases, planes, and other transportation.
Our haphazard urban planning and rise in domestic travelling further exacerbated the situation, leading mosquitoes to spread as epidemic vectors.
The ideal external temperature for Aedes breeding is 25-29.5 degree Celsius at 80% humidity. When there is a rise of temperature to 32 degree Celsius to 35 degree Celsius, the mosquitoes develop faster, the virus within the mosquitos replicate rapidly and the biting rate of the vector becomes higher, which results in swifter disease transmission.
This might explain the earlier than usual disease spread this year since we recorded the hottest summer from April through July with just the right amount of rainfall to create the perfect setting for a disease outbreak.
Why is it important to identify the dominant variant and treatment protocol?
There are four distinct serotypes of the dengue virus. Recovery from infection by one of these four (DEN-1, DEN-2, DEN-3, and DEN-4) provides the infected person with lifelong immunity against that particular strain and cross-immunity for six to 12 months to the other serotypes. If the person is infected by other serotypes subsequently then the risk of severe dengue increases.
The Institute of Epidemiology, Disease Control and Research must duly identify the dominant variant of the season and announce it to help individuals remain aware of what they were struck with. The symptoms of the disease are altering with each passing year; therefore, treatment protocol is also changing. This must be widely shared to avoid critical outcomes.
Can any strategic tool help in controlling vector breeding?
The Directorate General of Health Services (DGHS) maintains a dengue dashboard that updates the number of total cases in a day; they also publish a detailed press release of hospitalized dengue cases and deaths from all over the country. This same platform can be made interactive with real time reporting to take faster decisive actions.
Either the DGHS or the city corporations with the permission of the Ministry of Local Government, Rural Development and Co-operatives needs to set up a hotline number or an app or any other platform where hospitals and the diagnostic laboratories are mandated to report the present home addresses and particulars of all active dengue positive patients. This information can feed into a geographical information system (GIS) that creates a heat map for visualizing the locational statistics of the disease infested areas.
Once the heat map generates the exact location of the source of disease, the authorities can inspect the areas, find and clean the reservoirs, calculate 400m radius of the areas to intensely destroy not only the mosquitoes but the eggs and the larvae too till the outbreak is under control. Simultaneously short video clips of the eggs, larva, and the breeding containers must be widely distributed within communities for general citizens to actively participate in cleaning their surroundings.
A national daily recently reported on neighbouring West Bengal’s successful strategy, conceived as far back as 1985, where the foundation was laid by first understanding the nature of the mosquito. They have set up one committee for each ward that consists of the local councilor, one doctor, local citizens, and the vector control officers. Their main strategy is to find the source and eliminate it.
An enriched data repository of the addresses of homes and offices where larvae were found is maintained and the city corporation cleaning bill is added to the income tax of the landowner as a fine. There are two more level layers of vector control authorities that consist of entomologists, doctors, and vector control officers to monitor this program.
The Bangladesh local government is divided into city corporations/pourashovas in the urban areas which are again divided into wards. Elected mayors are the heads of city corporations, and councilors are the elected representatives from the wards. In rural areas, districts are divided into upazilas which are constituted by unions. Every union is divided into nine wards with elected members representing the wards, and the chairman of the union heads the council of the members.
The city corporations are vested with the public health, public welfare, and public works functions delegated to them by the Local Government Act 2009. The mayors have the executive power of city corporations and are the head of all the councilors. Dhaka South City Corporation has 75 general and 25 reserved women ward councilors and Dhaka North City Corporation has 54 general and 18 reserved women ward councilors.
Can we not utilize these elected leaders, make similar committees as West Bengal to drive a knowledge-based vector control strategy? This requires real dedication, tactical planning, and a goal to eliminate the disease from the source. Even if the GIS heat mapping is deemed expensive, a simple tool of hotline number connected to all the committee heads can inform them to take instant action.
What is the role of citizens?
Be aware. Understand the enemy and control the spread till a vaccine is invented. Even one death is too many given that we have had 23 years to understand the vector and disease spread. Videos, leaflets, text messages with photos of the mosquito, its eggs, its larvae, and the breeding sites must be widely broadcast to all levels of citizens via tv, radio, and social media. If dengue infested specific zip codes are identified, then people living in those areas must be alerted via text messages to clean up their neighbourhood. A diligent pest control system is needed at the ports to avoid migration of vectors.
Marigold, eucalyptus, mint, lemongrass, grapefruit, lavender, and pine oil all repel mosquitoes. We can cultivate some of these trees in our surroundings. Use of mosquito repellents, wearing light coloured loose fitted clothes covering the full body, and sleeping under mosquito nets will offer some protection.
Experimental projects such as using genetically modified sterile male mosquitoes and the use of Wolbachia bacteria to inhibit the replication of dengue virus within Aedes to suppress dengue transmission have been much in discussion but yet to be executed. It is time that at least a pilot project is launched.
It is undeniably a major health disaster with more than 46,495 cases and 303 deaths till now this year where children are suffering the most. Over the last 24 hours until Saturday, 10 more deaths were recorded due to dengue. Can we not study the successful strategies developed around the world and make some drastic actionable long-term and short-term plans to mitigate this menace?
Dr Maliha Mannan Ahmed is the Founder and Executive Director of Organikare. She has an MBBS, MBA, and a Master’s in Health Care Leadership.
Source: Dhaka Tribune.